FIU researchers from across disciplines have concerted efforts during the COVID-19 pandemic. From creating programs that track the virus’s spread to examining the efficacy of emerging telemedicine technology among underserved communities, and more, their work seeks to advance understanding of the novel virus that has infected more than 52.9 million people worldwide.
Their projects are informing policymakers and health care professionals, as well as the community, and have been supported by multiple federal grants and other programs. Here is just a handful:
Tracking COVID-19’s spread throughout Miami-Dade County
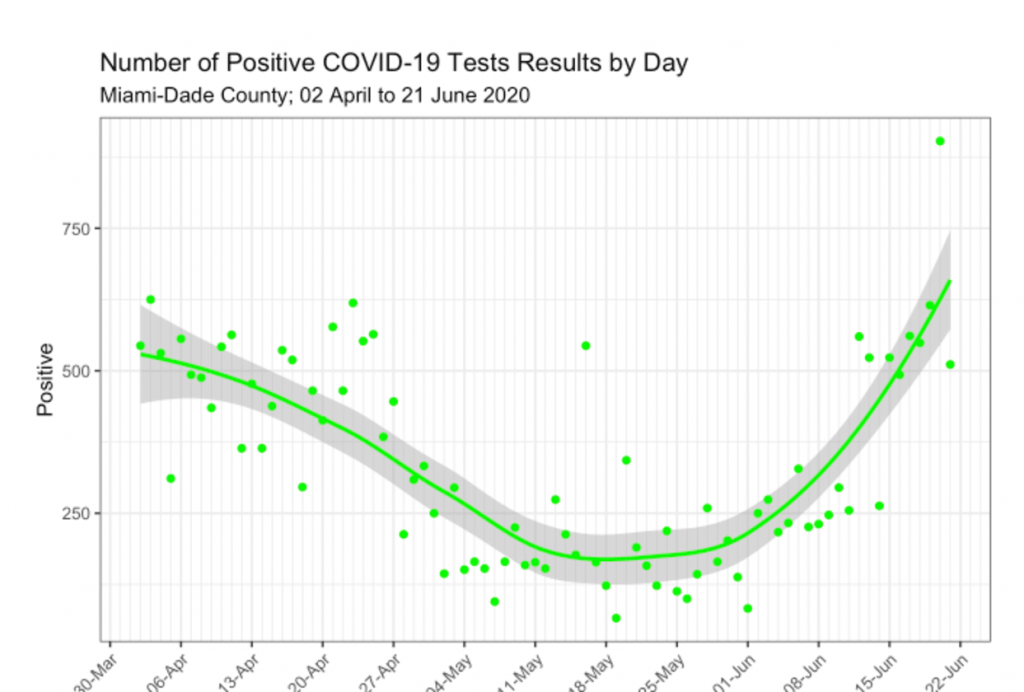
Researchers from FIU’s Robert Stempel College of Public Health & Social Work have launched the Miami-Dade COVID-19 Trend Tracker, a website dedicated to monitoring the long- and short-term trends of COVID-19 and its impact on local hospitals. They have been working with municipalities and their administration throughout Miami-Dade County to educate policymakers as the county is experiencing a resurgence of cases within the first COVID-19 wave.
The website, which is publicly available, tracks long- and short-term trends of COVID-19 data throughout the county since April 2 as well as hospitalization data, a key indicator of the county’s hospital capacity to handle existing and new cases. This is the only tracker specific to South Florida and, unlike the health department website, the tracker reports the average change over time.
Researchers: Zoran Bursac, chair of the Department of Biostatistics; Mary Jo Trepka, chair of the Department of Epidemiology; Gabriel J. Odom, assistant professor of Biostatistics; and Roy Williams, recent Stempel College biostatistics graduate
Examining use of telemedicine among vulnerable communities in South Florida

Dr. Sahar Ajabshir of the Herbert Wertheim College of Medicine received a $50,000 grant from the Center for Research on U.S. Latino HIV/AIDS and Drug Abuse (CRUSADA) to examine use of telemedicine among vulnerable communities during the pandemic.
The study is a partnership between FIU and a community-based primary-care clinic that provides free health care services to low-income, uninsured members of the South Florida community.
“Considering the higher prevalence of underlying medical conditions among minority and socioeconomically disadvantaged communities, and the loss of employer-based insurance among the millions who have lost their jobs, it is imperative to find a solution to maintain and expand access to health care for these communities in South Florida as we expect the second peak of COVID-19 pandemic during the upcoming fall and winter,” says Ajabshir.
One such solution is telemedicine (virtual, remote visits with health care professionals), which has long been utilized as a convenient tool to provide health care. Use of telemedicine has increased greatly during the COVID-19 pandemic, and it has the potential to broaden health care access; but Ajabshir says not much is known about the racial/ethnic and sociodemographic differences in utilization of telemedicine among vulnerable populations in South Florida.
Mitigating impact on the health care system

A shortage of basic medical supplies, personal protective equipment (PPE) and medical technology has been a major challenge for health care professionals around the world. Researchers from the College of Engineering & Computing (CEC) and the College of Communication, Architecture + The Arts (CARTA) saw the immediate need to build upon existing platforms to help the health care system and address the shortage.
With an NSF RAPID award, the researchers will create a mobile app, using artificial intelligence and augmented reality, as a digital “hub” for PPE training. In addition, the platform will support innovation and the manufacturing of essential medical equipment through the element of networking, where end users can connect with manufacturers.
Contact tracing and the science of memory

FIU researchers are studying how to improve contact tracing by tapping into people’s memory. Psychologists Deborah Goldfarb, Jacqueline Evans and Ronald Fisher are leading a new study funded by an NSF Rapid Response grant to identify a more effective way to conduct contact tracing.
The FIU team will test whether memory for contacts can be improved across different age ranges. Specifically, this study will test whether people between the ages of 9 and 90 recall more contacts when questioned using the cognitive interview compared to a standard contact tracing interview.
The cognitive interview was originally developed by Fisher to gather information from witnesses to crimes. It applies theories of social and cognitive psychology to increase the amount of information a person remembers during an interview. This technique is considered by many to be the gold standard in investigative interviewing. Now, it is being used to improve contact tracing and help flatten the curve of COVID-19.
Addressing COVID-19 impact on African Americans

COVID-19 is hitting the Black community hard. Early data from the Centers for Disease Control and Prevention suggest that African Americans are more likely to get infected and die from the new coronavirus. Dr. Cheryl Holder, an associate professor at the Herbert Wertheim College of Medicine, is spearheading an effort to address the impact of COVID-19 on African Americans in Florida.
“I know first-hand how African-American communities are disproportionately affected by whatever is taking place in society at large. COVID-19 is no different,” she said. Holder, an HIV specialist, is a veteran of the battle against AIDS. That experience is causing her extreme concern about the effects of the current epidemic on minority communities.
It is well known that African Americans have high rates of some of the underlying conditions that make COVID-19 more lethal. “African Americans are 2.2 times more likely to have diabetes, 20 percent more likely to have high blood pressure, 30 percent more likely to be obese, more likely to have HIV, asthma and sickle cell anemia and more likely to live in poverty… All of these underlying health conditions put African Americans at a greater risk of death if they contract COVID-19,” she wrote in an OpEd for The Miami Herald.